Topics:
Introduction
Stay in the loop with the latest news and updates from Serefin Health through our quarterly newsletter, SerefinRx. Whether you regularly engage with our team or have no immediate health concerns, keeping up to date on current health information empowers you to make informed decisions that benefit your well-being. Packed with valuable information, each issue offers a wealth of content, including company updates, health education, and much more.

About us
At Serefin Health, our primary focus is the well-being of our clients, and we are committed to going above and beyond to ensure the quality of your care and your satisfaction.
Our knowledgeable team of healthcare professionals is at the core of our service. With their unwavering dedication and expertise, they work collaboratively to provide compassionate and empathetic care that addresses your unique needs.
.jpg)
We take great pride in advocating on your behalf and strive to empower you to take an active role in your health and well-being, providing you with the knowledge and resources necessary to make informed decisions about your health. We are here to support and guide you every step of the way.
We foster a culture centered around teamwork and a shared commitment to finding innovative solutions to complex problems. By promoting continuous learning and improvement, we stay at the forefront of advancements in the field, enabling us to provide you with the highest quality of care.
May MS Awareness Month: Understanding, Supporting, and Connecting
May is Multiple Sclerosis (MS) Awareness Month in Canada, a time to learn, share, and stand together in support of the over 90,000 Canadians living with MS. This month, we spotlight the challenges of MS, the resilience of those affected, and the vital role of caregivers and communities in fostering hope and connection.
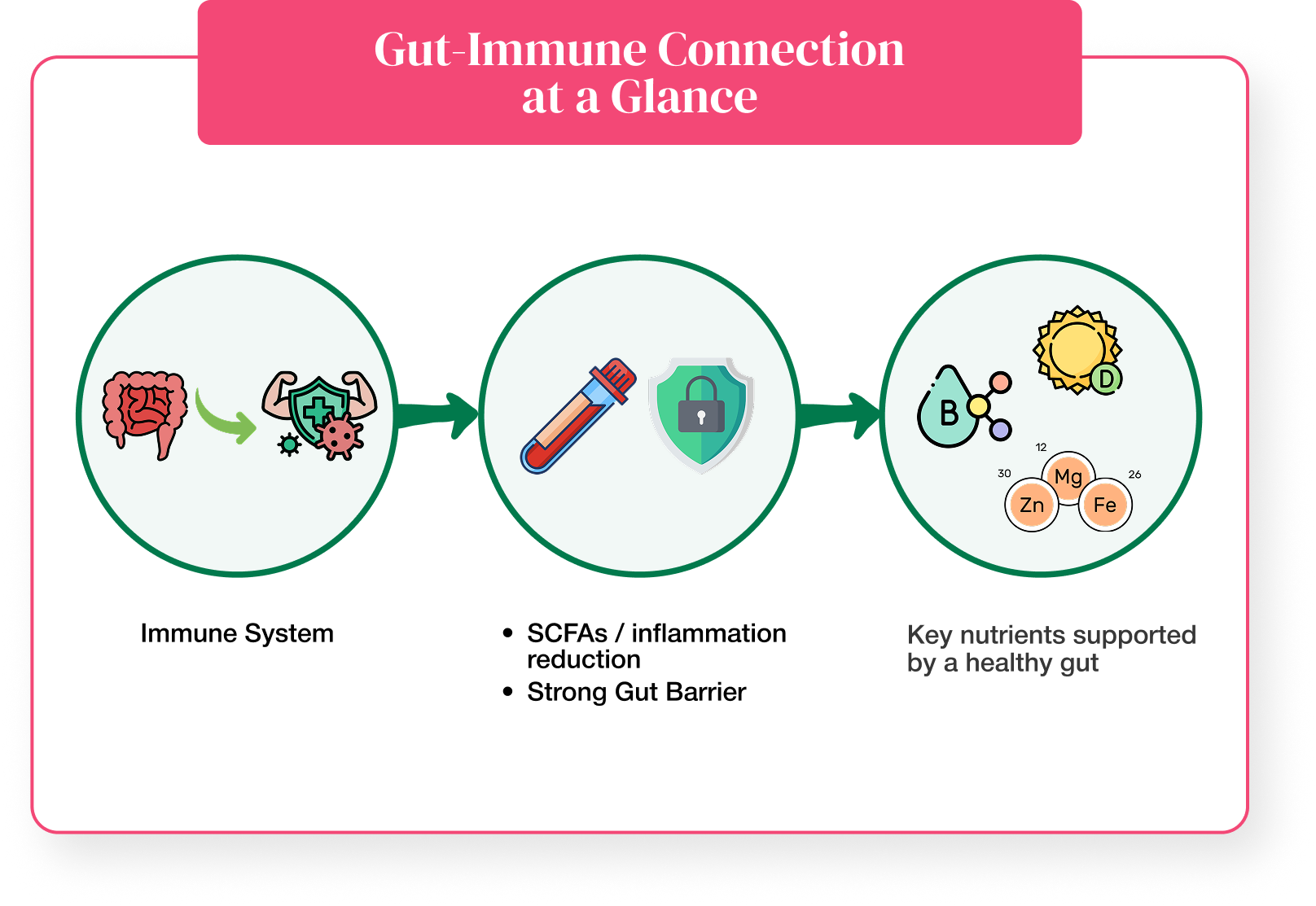
What Is MS?
MS is a chronic autoimmune disease that affects the central nervous system, including the brain, spinal cord, and optic nerves. It disrupts the protective sheath (myelin) around nerve fibers, causing inflammation and often leading to permanent damage or deterioration of the nerves themselves.
MS is unpredictable and can progress in different ways, making each person’s experience unique. In Canada, women are three times more likely to be diagnosed than men, and the average age of diagnosis is 43.
Symptoms and Impact
The symptoms of MS are often unpredictable and can affect physical, emotional, and cognitive functioning. Some of the most common symptoms include:
- Fatigue (experienced by about 80% of people with MS)
- Numbness or tingling, especially in the limbs
- Muscle weakness or spasms
- Difficulty with balance and coordination
- Blurred or double vision
- Memory and concentration challenges (sometimes referred to as "cog fog")
In some cases, MS can be mild and manageable; in others, it can lead to significant disability over time. The course of the disease also varies, and some people experience periods of relapse and remission, while others have a more progressive form of MS.
Diagnosis and Treatment
Diagnosing MS can be complex, and it involves a combination of neurological exams, MRI scans, and sometimes spinal fluid analysis. There is currently no cure for MS, but there are numerous disease-modifying therapies (DMTs) available in Canada that can help reduce the frequency and severity of attacks and slow disease progression.

New treatments and approaches are emerging all the time, thanks in large part to research supported by organizations like the MS Society of Canada. These therapies, along with lifestyle changes, physical rehabilitation, and mental health support, can make a big difference in quality of life.
Support for Caregivers
Caregiving is a cornerstone of MS care, yet it often goes unrecognized. Whether you are a spouse, parent, child, or friend, your role is vital and challenging. Caregivers often juggle tasks like managing appointments, providing transportation, assisting with daily activities, and offering emotional support.

The MS Society of Canada offers several resources to support caregivers:
- 1:1 Peer Support Program: Connect with trained volunteers who have lived experience with MS caregiving.
- Virtual Caregiver Peer Support Group: Join a nationwide group every second Sunday at 3:00 PM ET to share experiences and strategies.
- Caregiver Podcast: Listen to real stories about the emotional and practical aspects of caregiving.
- We Talk MS: Mentoring program that provides education, resources, and community connections for people living with multiple sclerosis and their families.
Some Interesting Facts About MS in Canada
- Canada has one of the highest rates of MS in the world
- On average, 12 Canadians are diagnosed with MS every day
- MS is the most common neurological disease affecting young adults in Canada
- Over 75% of people living with MS in Canada are women
How You Can Get Involved
- Educate Yourself: Visit MS Canada to learn more about MS, its symptoms, and the latest research.
- Advocate: Join the #TakeActionForMS campaign by sending a letter to your Member of Parliament, urging them to prioritize MS research funding.
- Participate: Engage in local events or virtual gatherings to raise awareness and support the MS community.
You Are Not Alone
Whether you are living with MS or supporting someone who is, remember that help is available. The MS Canada offers a range of services, including information, support, and educational events, to assist individuals and families affected by MS.
If you or someone you know is living with MS and would like to learn more, or simply talk about your experience, please do not hesitate to reach out to the Serefin Clinic Team. We are here to provide support, guidance, and information to help you navigate your health journey.
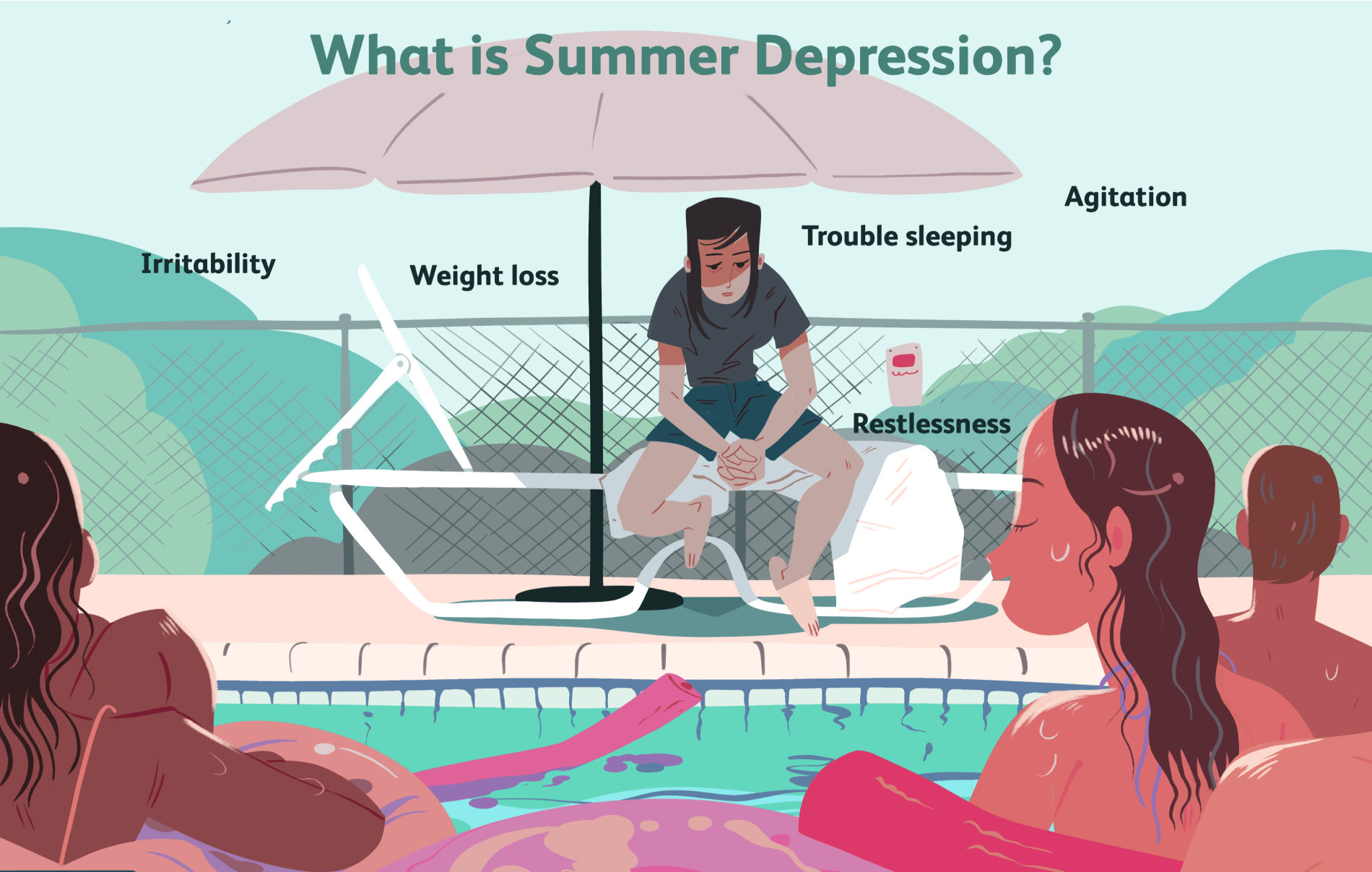
Summer Depression: The Hidden Struggles of the Sunny Season
While most associate depression with cold, dark winters, summer can also trigger a lesser-known form of Seasonal Affective Disorder (SAD). For some, longer days, heat, and heightened activity levels can bring on feelings of fatigue, anxiety, and disconnection.
What Causes Summer Depression?
Triggers vary, but common culprits include:
- Heat & Humidity: that can be physically and emotionally draining.
- Disrupted Routines: vacations and schedule changes can increase stress.
- Sleep Issues: long daylight hours interfere with natural sleep cycles.
- Overstimulation: social demands and travel may cause burnout.
- Hormonal Changes: fluctuations in serotonin levels may impact mood.
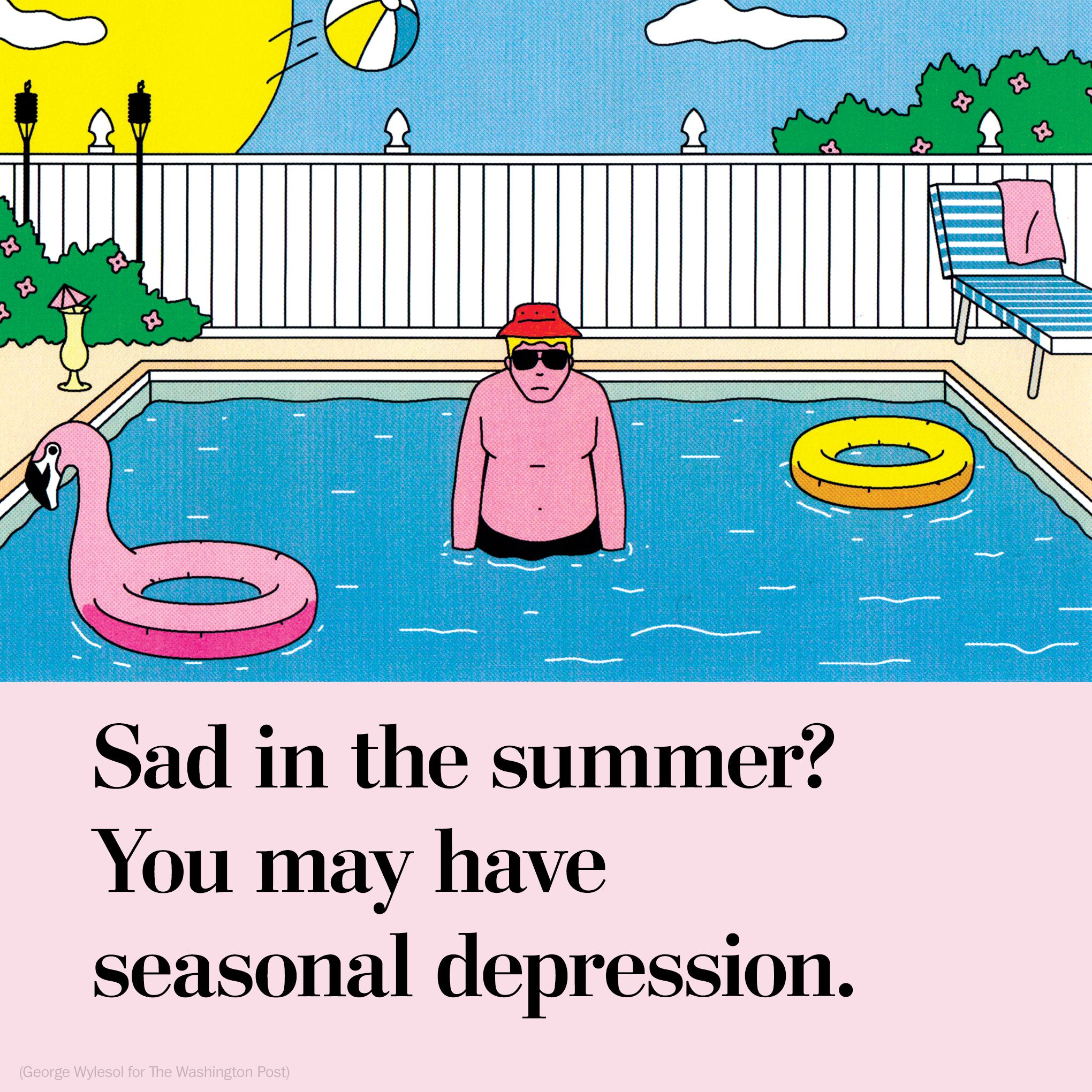
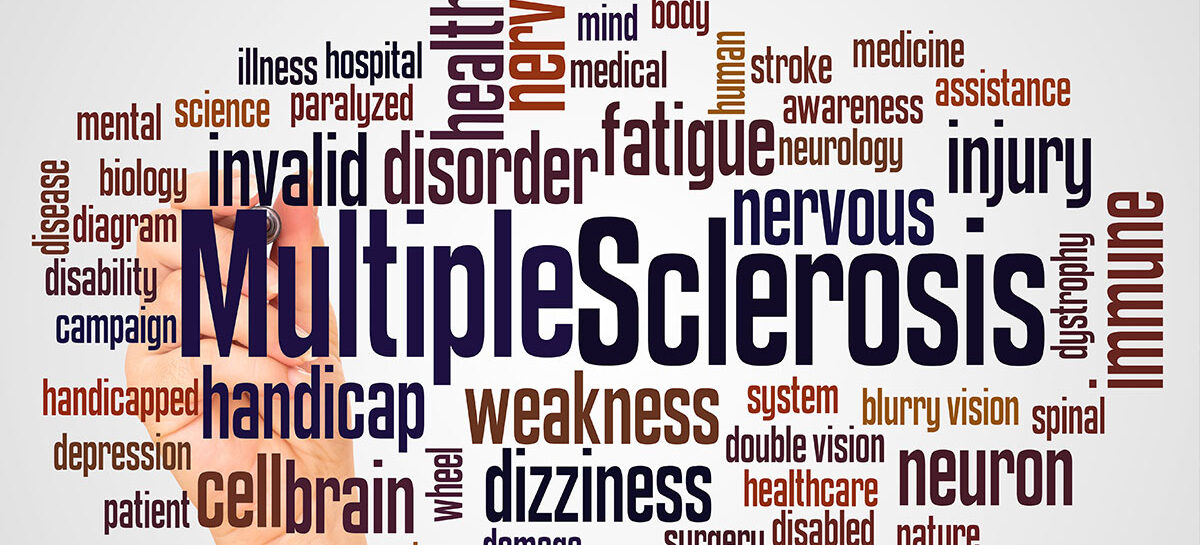
What Are the Signs?
Symptoms of summer depression can include:
- Insomnia
- Irritability
- Loss of appetite
- Increased anxiety
- Restlessness
- Difficulty concentrating
- Tendency to withdraw socially.
Unlike winter depression, it is often a quiet, internal battle that can feel confusing and isolating.
How to Cope?
- Therapy: Cognitive Behavioral Therapy (CBT) can help shift negative thought patterns.
- Vitamin D: get safe sun exposure early or late in the day - supplements may help.
- Stay Cool: hydrate, use fans or AC, and try cool baths to manage heat.
- Mindfulness: practice yoga, meditation, or deep breathing to calm anxiety.
- Routine: keep consistent sleep and meal times to reduce stress.
- Limite Alcohol: alcohol can worsen symptoms and disrupt sleep.
- Medication: SSRIs may be indicated. Consult a doctor if symptoms persist.
When to Seek Help
If symptoms interfere with daily life or you experience thoughts of self-harm, reach out to a mental health professional immediately. You're not alone, and help is available.
Take Back Your Summer
Summer depression is real, but manageable. With the right tools and support, you can restore balance and find peace - even on the sunniest of days.
Sodium: Salt Intake and How It Affects You
Table salt (sodium chloride) is a fundamental part of our diet, playing a key role in fluid balance, nerve function, and muscle contractions. However, excessive sodium intake is a leading contributor to high blood pressure, heart disease, and other serious health concerns.
So how much salt is too much? And what steps can we take to maintain a healthy balance? Let’s break it down.
The Role of Sodium in the Body
Sodium is an essential mineral that helps regulate:
- Fluid Balance – It controls how much water the body retains or excretes.
- Nerve Function – It ensures that nerve signals are transmitted correctly.
- Muscle Contraction – It helps muscles (including the heart) contract properly.

But while we need sodium to survive, most people consume far more than their bodies require.
The Recommended Daily Intake vs. Reality
Health Canada recommends no more than 2,300 mg of sodium per day (about one teaspoon of salt), with an ideal limit of 1,500 mg per day. However, the average person consumes over 3,400 mg daily—far exceeding the recommended levels.
This excess sodium can contribute to:
- Hypertension (High Blood Pressure): Increased sodium causes the body to retain water, leading to higher blood volume and pressure on arteries. Over time, this increases the risk of heart disease and stroke.
- Kidney Strain: The kidneys must work harder to filter out excess sodium, which can lead to kidney disease or kidney stones.
- Fluid Retention and Swelling: High sodium intake can cause bloating and swelling in the hands, feet, and face.
Where Is All This Extra Salt Coming From?
It’s easy to assume that cutting back on table salt is enough, but over 70% of the sodium in our diets comes from processed and restaurant foods—not from the salt shaker. Common high-sodium culprits include:

- Processed meats (bacon, ham, deli meats)
- Canned soups and broths
- Packaged snacks (chips, pretzels, crackers)
- Frozen meals and fast food
- Condiments and sauces (soy sauce, ketchup, salad dressings)
- Even foods that don’t taste salty—like bread, cheese, and breakfast cereals—can contain significant amounts of hidden sodium.
How to Reduce Your Sodium Intake Without Losing Flavor
Lowering sodium doesn’t mean sacrificing taste. Here are some evidence-based strategies to cut back while still enjoying flavorful meals:
- Choose Fresh, Whole Foods – Opt for fresh fruits, vegetables, lean proteins, and whole grains instead of processed options.
- Read Nutrition Labels – Look for "low-sodium" or "no added salt" options, and compare brands to find those with less sodium. Even aiming for foods with less than 15% of your daily sodium intake per serving is a good place to start.
- Use Herbs & Spices – Replace salt with flavorful alternatives like garlic, lemon, vinegar, or fresh herbs such as basil, thyme, and rosemary.
- Rinse Canned Foods – Draining and rinsing canned beans and vegetables can reduce sodium by up to 40%!
- Cook at Home More Often – Preparing meals from scratch allows full control over sodium levels.
Final Takeaways
Salt is necessary for health, but moderation is key. By being mindful of hidden sodium sources and making small dietary changes, we can protect our hearts, kidneys, and overall well-being. A heart-healthy diet isn’t about restriction - it’s about making informed choices that benefit both immediate and long-term health.
If you have high blood pressure or other health concerns related to sodium intake, talk to your healthcare provider about personalized dietary recommendations.
Your health is in your hands - one mindful bite at a time.
Glycemic Index & Glycemic Load: What They Are and Why They Matter for Your Health
When it comes to eating well and feeling your best - whether you are managing diabetes, trying to lose weight, or just looking to stay energized carbohydrates play a big role. But not all carbs are created equal. Some carbohydrates can cause your blood sugar to spike high, while others give you steady, lasting energy.
This is where two important terms come in: Glycemic Index (GI) and Glycemic Load (GL). Understanding them can help you make smarter food choices without giving up your favorite meals.
First, What’s the Glycemic Index?
The Glycemic Index (or GI for short) is a way to rank how quickly carbohydrate-containing foods raise your blood sugar. It is a scale from 0 to 100, and the higher the number, the faster your blood sugar goes up after eating that food. For example, pure glucose - aka sugar has a GI of 100.
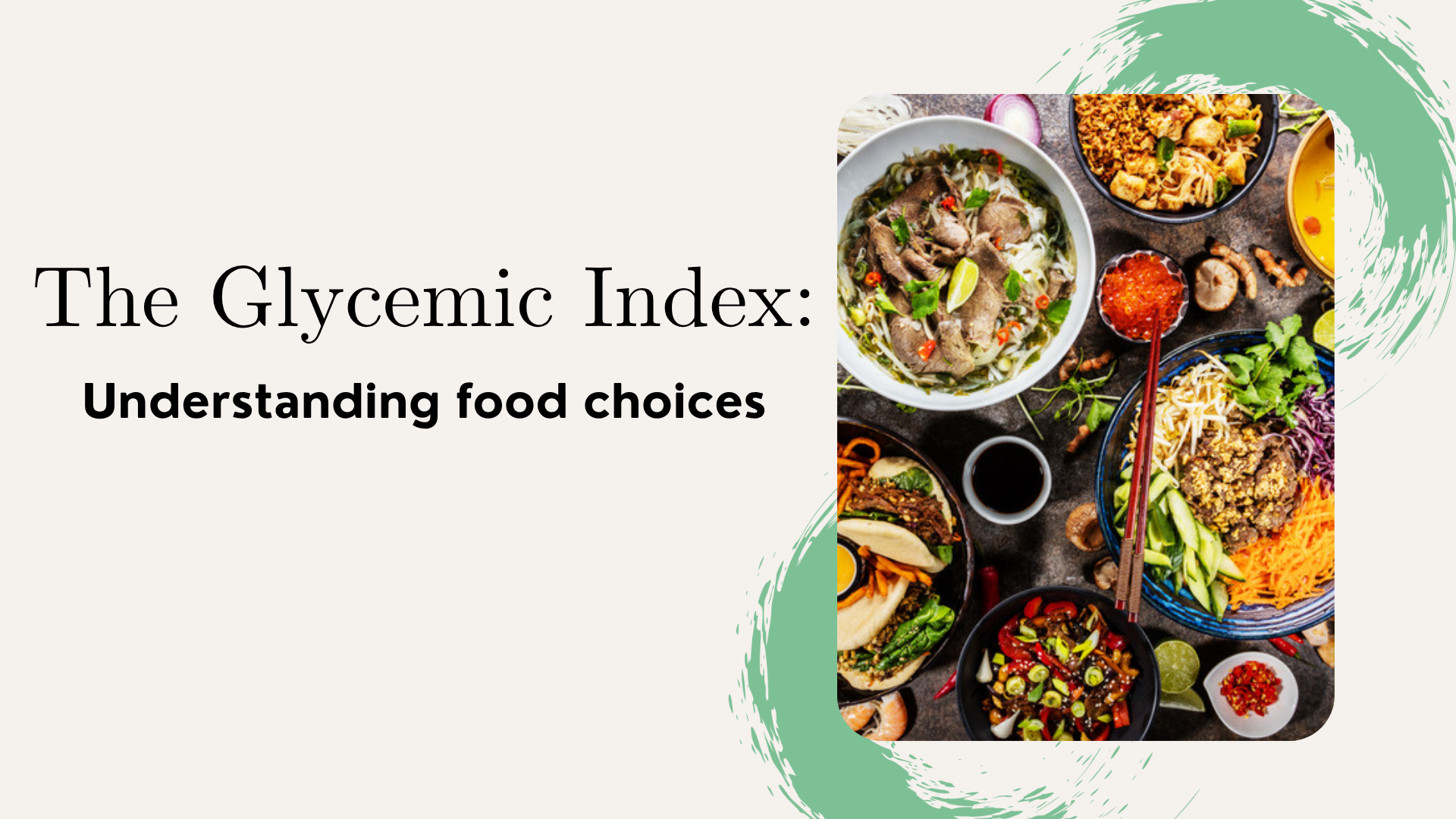
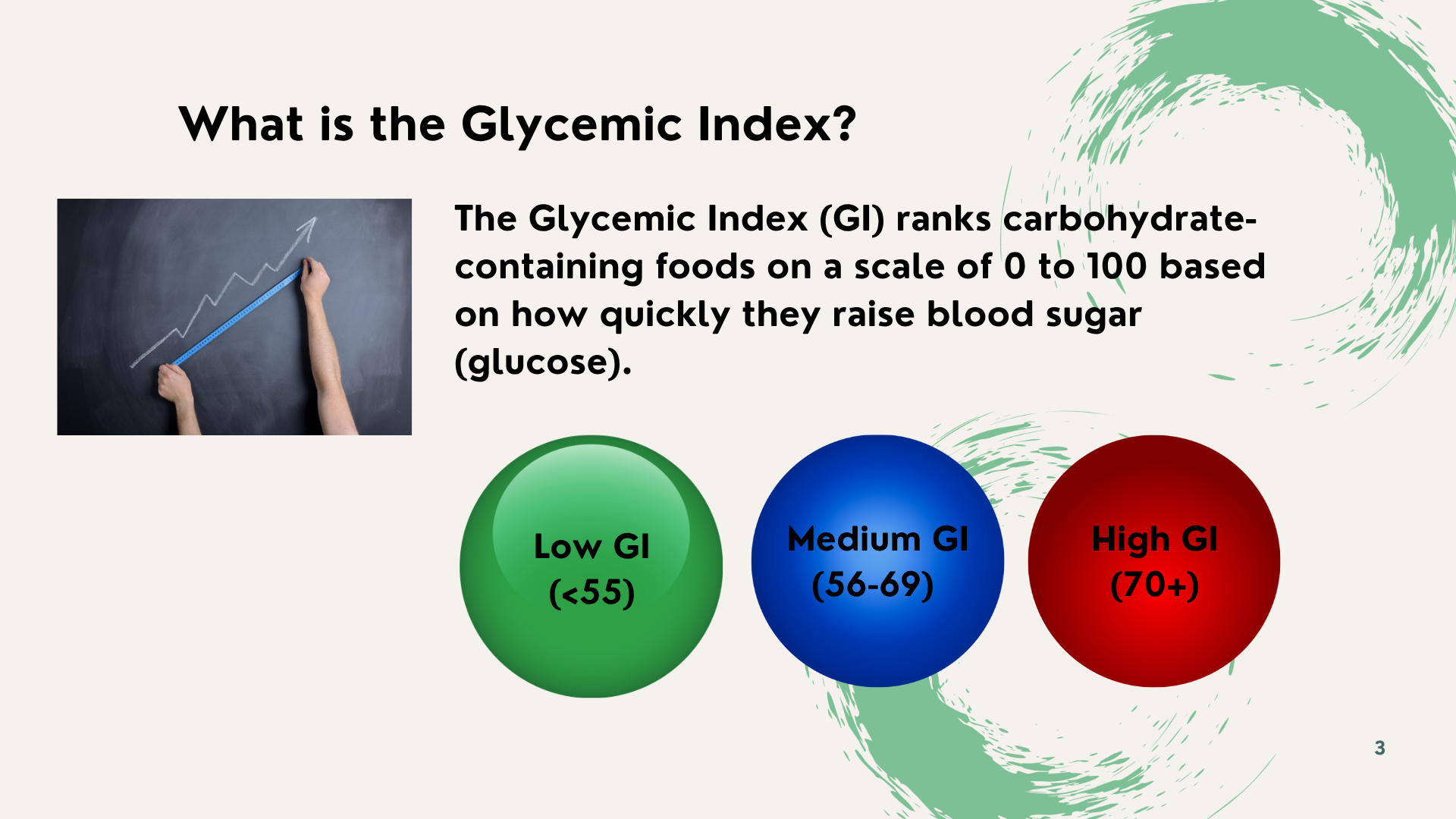
Here is the basic breakdown:
- Low GI (55 or less) = slower rise in blood sugar
- Medium GI (56–69) = moderate rise
- High GI (70 or more) = quick spike
Foods that are more processed tend to have a higher GI, while those with more fiber, fat, or protein usually land on the lower end.
But here is the catch: GI does not tell the whole story.
Why Glycemic Index Alone Is Not Enough
Just because a food has a low GI does not automatically mean it is healthy. And just because something has a high GI does not mean you should never eat it.
GI does not account for:
- Portion size – How much are you actually eating?
- Other foods on your plate – Do you have protein, fat, or fiber with it?
- How the food is cooked or processed – Cooking can change a food’s GI!
- How The type or ripeness of the food – A ripe banana has a higher GI than a green one. food is cooked or processed – Cooking can change a food’s GI!
And remember, GI only applies to foods with carbs. That means no GI score for foods like eggs, chicken, or olive oil. This is where Glycemic Load comes into play.
Glycemic Load (GL) takes things a step further. It factors in both how fast a food raises your blood sugar (GI) and how much carbohydrate is in a typical serving. In other words, it gives you the full picture of how food will affect your body.
So... What is Glycemic Load?

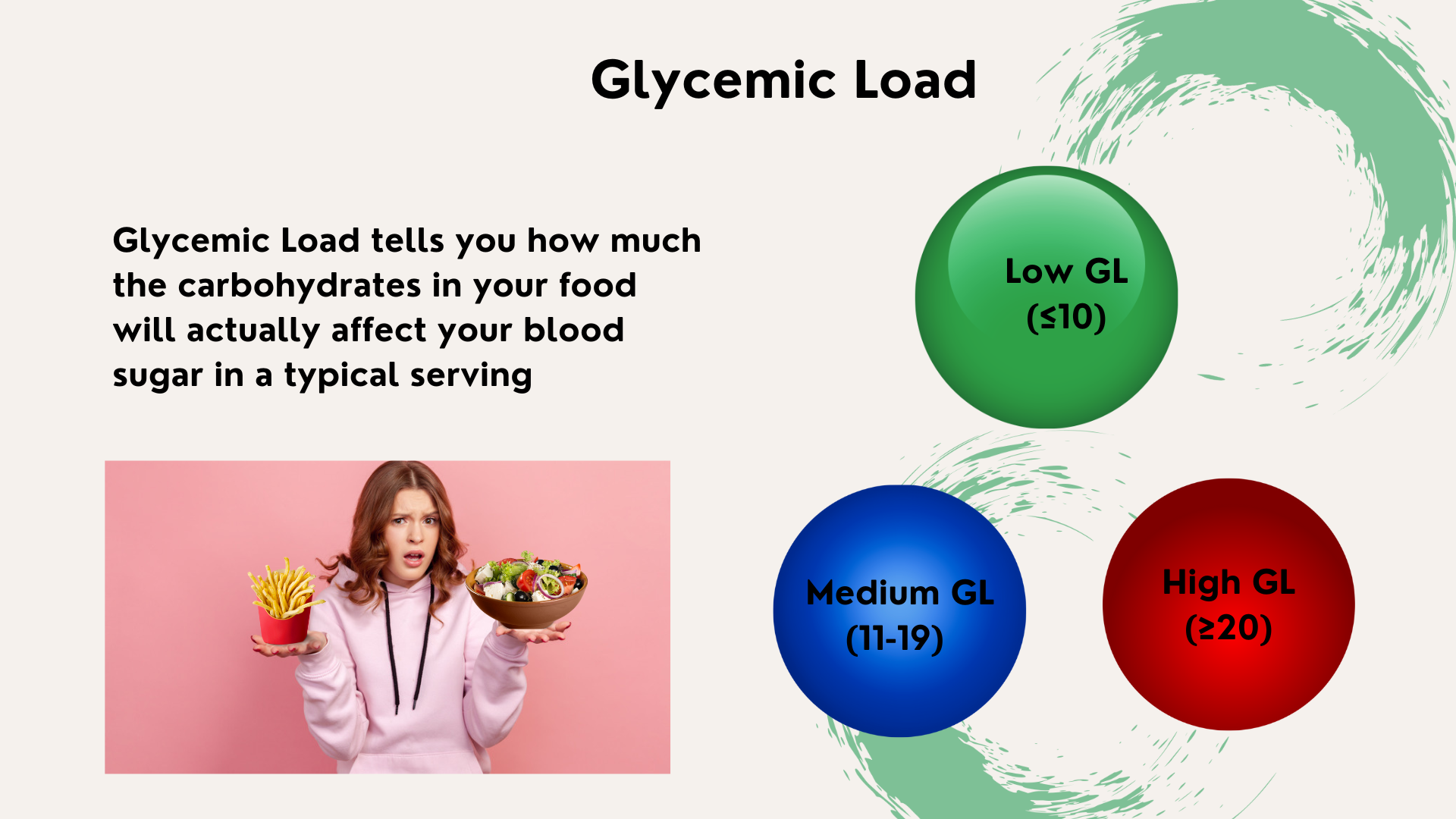
GL is broken down like this:
- Low GL (10 or less) = best for stable blood sugar
- High GL (20 or more) = likely to cause a spike
- Medium GL (11–19) = moderate effect
A Surprising Example: Watermelon vs. Doughnut
Let’s look at watermelon. It has a high GI of 76, which sounds bad but a typical serving only has 11g of carbs. So, its GL is low - meaning it will not spike your blood sugar as much as you might think.
Now compare that to a doughnut. Also, GI 76, but with 23g of carbs in a serving. That is a much higher GL, and a much bigger blood sugar spike.

Moral of the story? GI alone does not tell you how a food behaves in the real world. That is why GL is such a helpful tool.
So, What Should You Eat?
Here are some foods that are generally low in GL and great for keeping blood sugar stable and some high GL foods you should try to limit.
Low GL Food
- Vegetables and high-fiber fruits
- Beans, lentils, and chickpeas
- Whole grains like oats, quinoa, and barley
- Milk and plain yogurt
High GL Food
- White bread and white rice
- Sugary drinks and sweetened cereals
- Processed snacks and baked goods
And here is a smart trick: Pair carbs with protein or healthy fat (like nut butter, avocado, or eggs). This helps slow digestion and keeps blood sugar steadier.
Final Thoughts: Keep It Simple, Keep It Balanced
Do not stress about memorizing numbers or cutting out your favorite foods. GI and GL are just tools not rules to help guide your food choices. Focus on balance, variety, and how your body feels after eating.
If any of the information above feels overwhelming or unclear, remember that support is within reach. Our Serefin Clinic Team is here to guide you. Do not hesitate to reach out - we are here to support you every step of the way.
What Is New at the Clinic:
Meet Serefin Care Coordinators
We are pleased to announce the integration of Care Coordinators into our Serefin Clinic Team. As part of our commitment to delivering compassionate, patient-centered care, these team members are here to support patients in navigating their healthcare journey. Our Care Coordinators help ensure that each patient receives seamless and personalized support. We are excited to have them on board and look forward to the positive impact they will bring to your care experience.
Meet Serefin Care Coordinators:

Katie Vandenborre RN, Care Coordinator

Victor Karpov RN, Care Coordinator

Dragana Milivojevic RPN, Care Coordinator

Christine Turiano RN, Care Coordinator
With our patients always at the heart of what we do, we continually strive to enhance your experience and ensure you receive the highest quality of care. We are committed to supporting your health and well-being every step of the way.
We kindly request one minute of your time to complete this survey, as your answers will contribute to improving our Newsletter.
Start SurveyResources
May is MS Awareness Month: Understanding, Supporting, and Connecting
https://mscanada.ca/what-is-multiple-sclerosishttps://stories.northernhealth.ca/stories/unbc-volunteers-support-ms-clients-northern-bchttps://mscanada.ca/find-support/ms-support-groups/care-givers-ms-peer-support-grouphttps://www.verywellhealth.com/living-with-multiple-sclerosis-2440580https://mscanada.ca/about-mshttps://mscanada.ca/intro-to-ms/what-is-multiple-sclerosishttps://mscanada.ca/msawarenessmonthPicture sources:
https://www.kauveryhospital.com/blog/neurology/what-is-multiple-sclerosis-ms/https://msnz.org.nz/msnz-resources/msnz-what-is-ms-png/https://www.healthdigest.com/619386/multiple-sclerosis-explained-causes-symptoms-and-treatments/Summer Depression: The Hidden Struggles of the Sunny Season
https://www.normanrosenthal.com/blog/2023/06/reverse-seasonal-affective-disorderhttps://www.nimh.nih.gov/health/publications/seasonal-affective-disorderhttps://www.scientificamerican.com/article/summertime-depression-could-be-a-type-of-seasonal-affective-disorderhttps://www.psychiatrictimes.com/view/the-other-sad-summer-seasonal-affective-disorderhttps://www.healthline.com/health-news/seasonal-affective-disorder-can-affect-you-in-the-summer-toohttps://www.psychologytoday.com/us/blog/romantically-attached/202407/navigating-summer-seasonal-depressionhttps://www.forbes.com/health/mind/summer-depression-surveyhttps://arxiv.org/abs/2312.02953 https://arxiv.org/abs/2404.11212https://www.forbes.com/health/mind/summer-depression-survey/https://www.psychologytoday.com/us/blog/romantically-attached/202407/navigating-summer-seasonal-depressionhttps://www.scientificamerican.com/article/summertime-depression-could-be-a-type-of-seasonal-affective-disorder/https://prairie-care.com/summer-depression/ https://www.ncbi.nlm.nih.gov/books/NBK568745/ https://www.sciencedirect.com/science/article/abs/pii/S0165032723015380 https://www.healthline.com/health-news/seasonal-affective-disorder-can-affect-you-in-the-summer-too https://www.psychiatrictimes.com/view/the-other-sad-summer-seasonal-affective-disorderhttps://www.normanrosenthal.com/blog/2023/06/reverse-seasonal-affective-disorder/ https://www.renown.org/blog/10-facts-about-seasonal-affective-disorder https://www.pennmedicine.org/news/news-blog/2018/august/the-summertime-blues https://www.nimh.nih.gov/health/publications/seasonal-affective-disorder https://pubmed.ncbi.nlm.nih.gov/3688288/https://mhanational.org/conditions/seasonal-affective-disorder-sad https://www.camh.ca/en/camh-news-and-stories/summer-depression https://www.mayoclinic.org/diseases-conditions/seasonal-affective-disorder/symptoms-causes/syc-20364651Picture resources:
https://www.verywellmind.com/summer-depression-symptoms-risk-factors-diagnosis-treatment-and-coping-4768191https://www.bridgestorecovery.com/blog/5-tips-for-dealing-with-summer-depression/Sodium: Salt intake and how it affects you
https://www.canada.ca/en/health-canada/services/publications/food-nutrition/sodium-intake-canadians-2017.html https://pmc.ncbi.nlm.nih.gov/articles/PMC8030856/?utm_source= https://www.cdc.gov/salt/about/index.html?utm_source=Glycemic Index & Glycemic Load: What They Are and Why They Matter for Your Health
https://hopkinsdiabetesinfo.org/4-facts-you-should-know-about-the-glycemic-index/https://www.health.harvard.edu/diseases-and-conditions/the-lowdown-on-glycemic-index-and-glycemic-loadhttps://www.diabetes.ca/resources/tools-resources/understanding-the-glycemic-index-(gi)https://lpi.oregonstate.edu/mic/food-beverages/glycemic-index-glycemic-loadNavigating complexity, simplifying life.
© 2023 Serefin Inc. All rights reserved.

.png)
.png)
.png)
.png)
.png)







.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)
.png)






.jpg)
.jpg)


.png)

.png)
.png)